When children develop heart block, they often need a pacemaker, committing them to more operations, to maintain the pacemaker’s function, for the rest of their lives. Our ability to map the heart’s conduction system allows us to finally “see” where this tissue is located and give patients a vastly better chance of avoiding surgical complications, so they can focus on recovering from CHD treatment.
EP mapping also allows us to record the location of conduction tissue for further study. We’re finding that anatomical variables — like how a patient’s ventricles are arranged, where the heart is located inside the chest, and how the atria are oriented — can influence the location of the conduction system. While some of these findings were first discovered in older anatomy studies, our rapidly growing conduction mapping experience is enabling us to better understand where the conduction system is located across all variants of complex CHD.
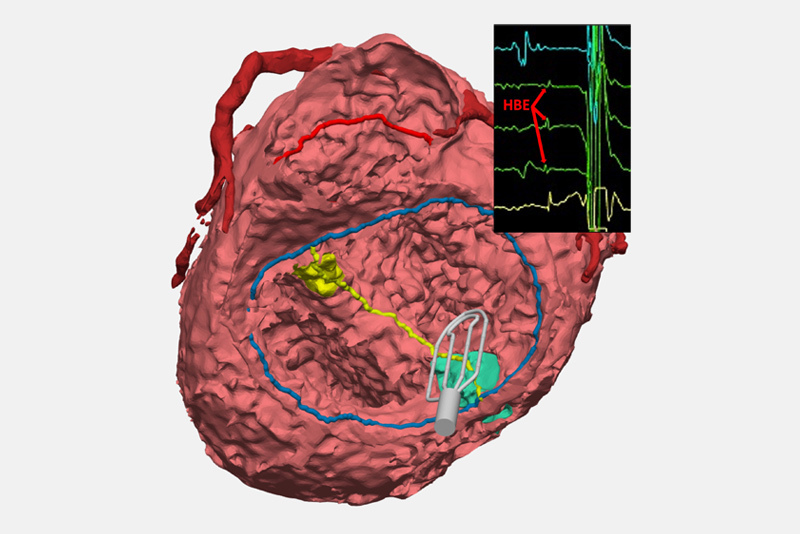
Our program is also creating 3-D models of the cardiac anatomies of every CHD patient who benefits from EP mapping in surgery. Ultimately, those individual models will be available in a digital library that will let clinicians review the influences that different anatomies have on conduction, which may help cardiologists and surgeons developed surgical plans informed by the conduction’s system location for each particular type of CHD.
Mapping conduction tissue is just the first of many innovations and collaborations we intend to pursue in the future, as we collectively work to better treat children with CHD and aim to reduce or eliminate altogether their risk of acquiring arrhythmia.